Azothioprine toxicity in a dog
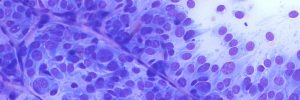
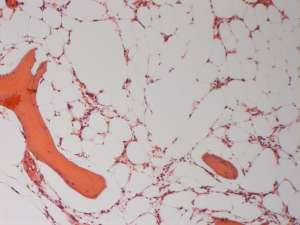
A five-year-old, male neutered Cavalier King Charles Spaniel developed a marked pancytopaenia whilst on prednisolone and azathioprine treatment for recurrent immune-mediated thrombocytopaenia. Bone marrow aspirates were of low cellularity and contained only low numbers of otherwise normal haematopoietic precursors. The following figures are of the bone marrow core.

Final Diagnosis
Marked megakaryocytic, erythroid and myeloid hypoplasia
Discussion
The marked hypoplasia of all three cell lines accounts for the pancytopaenia identified in the peripheral blood. This is not aetiologically specific. However, given the clinical/medication history, it is consistent with azathioprine toxicity. Within one to several months of initiating an immunosuppressive dose of azothioprine, neutropaenia, thrombocytopaenia or pancytopaenia can occur secondary to bone marrow hypoplasia/aplasia with or without myelofibrosis. Once the drug is discontinued, circulating cell numbers may slowly return to normal. Bone marrow cores in addition to bone marrow aspirates are helpful to confirm the presence of a truly hypocellular bone marrow (as opposed to a non-representative sample) and to assess for the presence of myelofibrosis.